
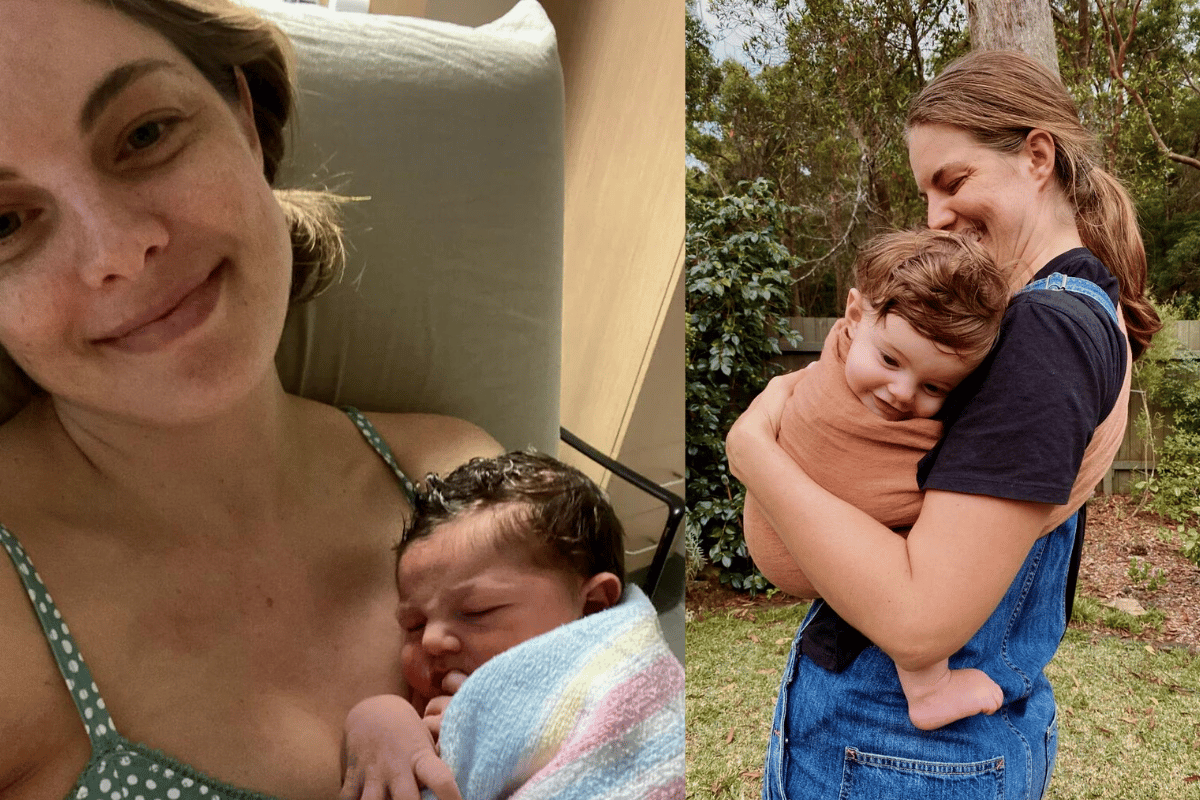
Proud Wiradjuri woman Jami had always dreamed of her birth experience reflecting her Indigenous culture.
One of the aspects she had been most looking forward to was a placenta burying ritual. It's a sacred act that is deeply significant within many cultures, including for First Nations people.
As the CEO of Victorian Aboriginal Community Controlled Health Organisation said, the premise is that the act of burying the placenta is telling mother earth and the country on which the child has been born to protect the new infant's spiritual soul.
With this in mind, Jami had plans to perform a placenta burial of her own. But after giving birth, Jami's placenta was thrown out by mistake.
And it had a major emotional impact.
Watch: Jessica Rowe on post natal depression. Post continues below.
Registered nurse Jami had been with her husband Tom for nine years when they started trying for a baby.
"I was very lucky to fall pregnant after four months," Jami said to Mamamia. "Especially as I had been told it might take longer because of my endometriosis."
Top Comments