
The survival rate can be as little as 15%.
It’s an idea most of us would take for granted. If you were unconscious, if you’d stopped breathing, you would want someone to use CPR. You would want them to resuscitate you.
Wouldn’t you?
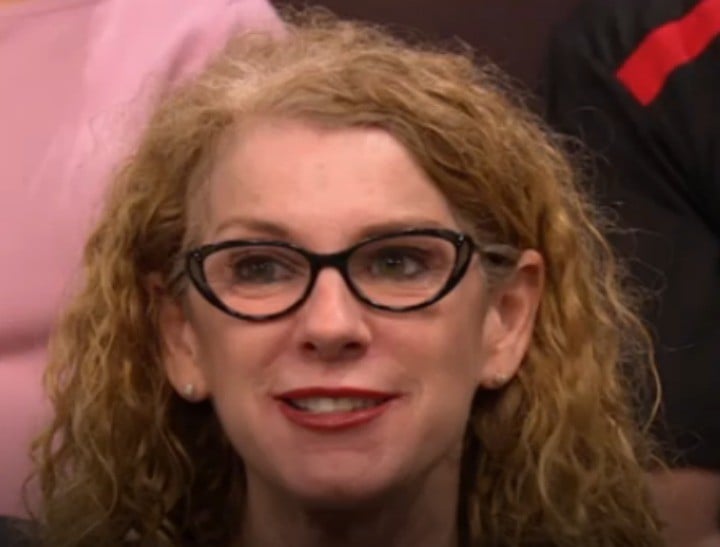
On last night’s episode of Insight on SBS, Jenny Brockie, along with a panel of experts and members of the studio audience discussed the notion that CPR is not always the best option.

Top Comments
How do you get a Do Not Resuscitate (DNR) order? Are they at a Federal or State level?
I don't have any tattoos, the only one I have considered was a simple DNR quote just above my breastplate, I don't know if that would be enough for medical staff to be legally protected by observing my wishes though.
It's something I've been thinking about since the Andrew Denton story on euthanasia.
You can get an Advance Health Directive which can outline all of your wishes for your health care. http://www.justice.qld.gov....
This is an example of one, just google it for your state.
A DNR order (which is called many different things in different hospitals including resuscitation plan) can be done with your medical team whenever you are in hospital. Make sure you discuss it with your family so they can let the doctors know if you are too unwell to communicate your wishes.
As for collapsing on the street I am not sure a tattoo would be taken seriously by first responders, unless under it there was "seriously! Check my bag for my advance health directive"
Will do. Thank you for the information Sarah, I really did not know these things existed. And I might need to get a new tattoo!
I wanted to ensure my wishes were observed without putting the medical staff in some sort of ethical or legal minefield.
They would probably resuscitate you regardless. No trained professional could ignore an opportunity to act. Damned if you do, damned if you don't.
in hospital once its clear there is a NFR order everything stops. In the street or ambulance it would be different and they probaply would resuscitate you