
I had so many strange questions before I got my tubal salpingectomy and I discussed them pretty openly with the people around me.
One night over the holidays I was sitting with my partner and my dad at a bar and were all talking about how interesting and unusual it was.
“So they take out the whole tube?”
“Yes, the whole tube. No fallopian tubes.”
“Where do… the eggs go?”
“Probably just like, into your body? They’re really small.”
“No, that can’t be right.”
Turns out, it was right. Your body does keep producing ova after the procedure, and they just kind of get spit out and dissolve.
All the annoying things people who don’t want kids have ever heard. Post continues after.
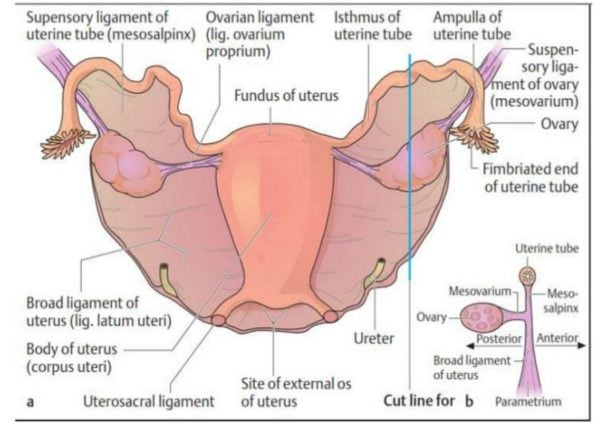
Over the month between when I finally got approval for elective sterilisation and when I actually had the procedure done, I learned more about my reproductive organs than in any sex ed class or My Body, My Self-esque book.


Top Comments
My husband's sister in law had to try to convince doctors she wanted this done not because she did not want children. She wanted no more of them, having four children and being in her very early 20's, she had enough of having children. The doctors excuses were what if you wanted more children, really it is the woman's choice.
For the modern time, a time that’s ‘supposedly’ more equal, the second a woman speaks up to the wrong Dr about her OWN uterus they have their opinions flying left right and center. It’s sad that it’s still at a point of having to ‘convince’ professionals on what you want for you own body.
Guys get those questions too.
I did, all my friends did.
It's standard to ask them.
I’m glad you did what suited you. You are right, it’s your body and your choices.