This post discusses addiction and distressing topics, and could be triggering for some readers.
Even as a young child, Ange never really felt like she fit in.
By the time she reached her 20s, she found alcohol to be "an excellent social lubricant".
"It [allowed me] to loosen up a lot, and I could talk to people," she shared on a recent episode of Mamamia's daily news podcast, The Quicky.
By her early 30s, Ange’s drinking increased; extending beyond weekends and stretching into weekdays.
Listen to the full interview with Ange below. Post continues after podcast.
And then it spiked further at 32, when Ange’s mother was diagnosed with brain cancer.
"I was just trying to drink the pain away."
Fourteen months later, Ange’s mother passed – and her alcohol consumption "progressed really quickly to 24/7, top-up drinking," she told The Quicky.
"This was compounded further when I was told after significant testing, without IVF, we had zero chance of having a baby."
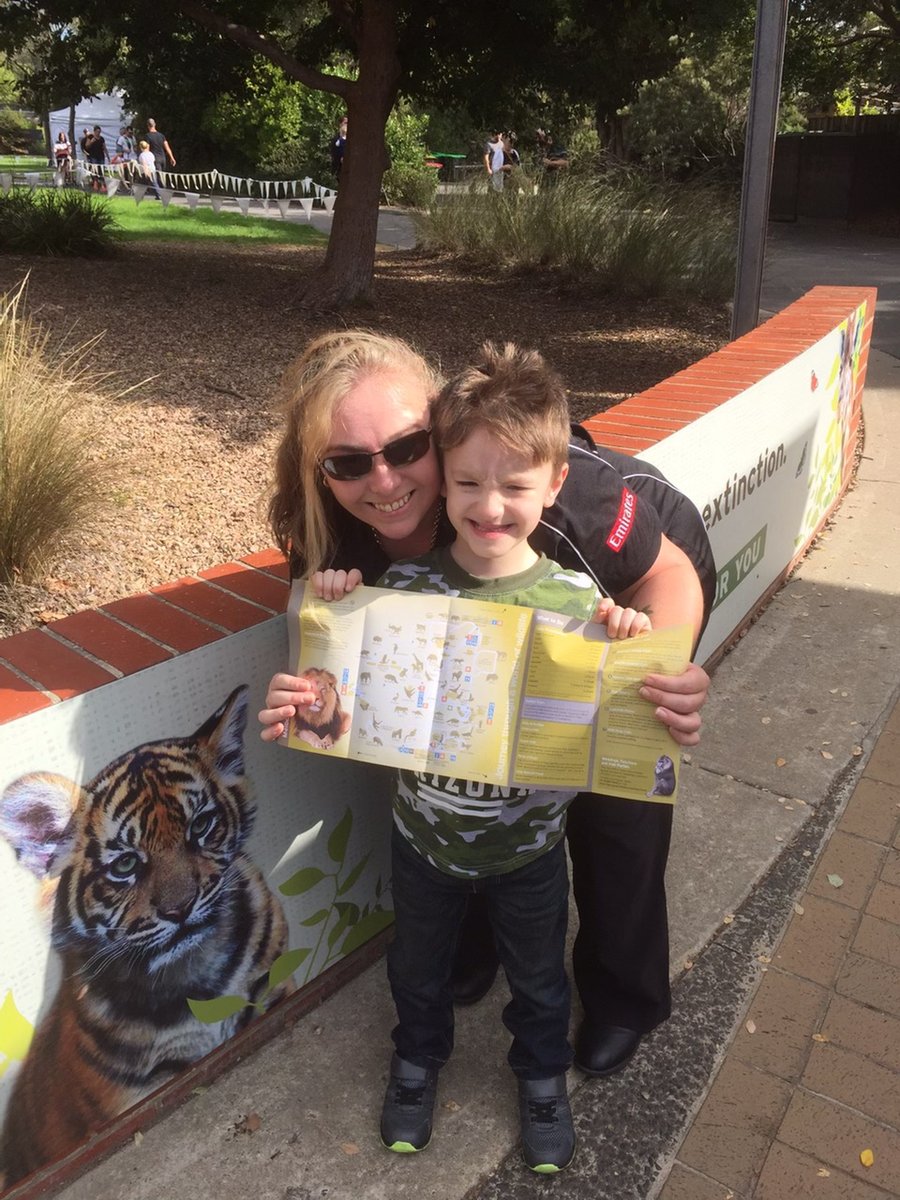
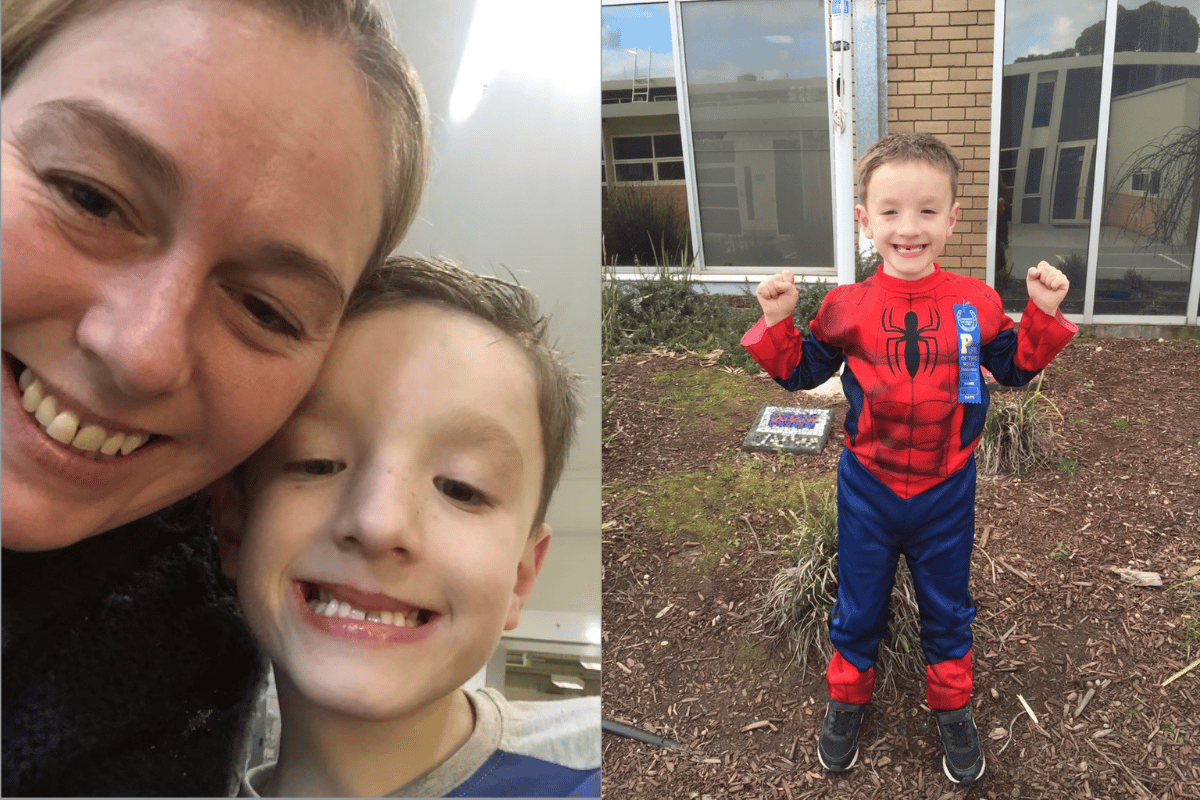
But at 35, Ange fell pregnant with her "miracle baby".
"I was absolutely elated. Unfortunately, that elation quickly turned to sheer horror as I realised the implications of my physical dependence on alcohol would be both on myself and more importantly, my baby," she shared.
"That was the horror moment of the whole thing, and that was when I realised that I couldn’t just stop drinking."