On Thursday evening, Prime Minister Scott Morrison gave a snap press conference in which his Government announced a significant change to Australia's COVID-19 vaccine rollout plan.
Based on advice from The Australian Technical Advisory Group on Immunisation, it's now recommended that Australian's under the age of 50 receive the Pfizer vaccine.
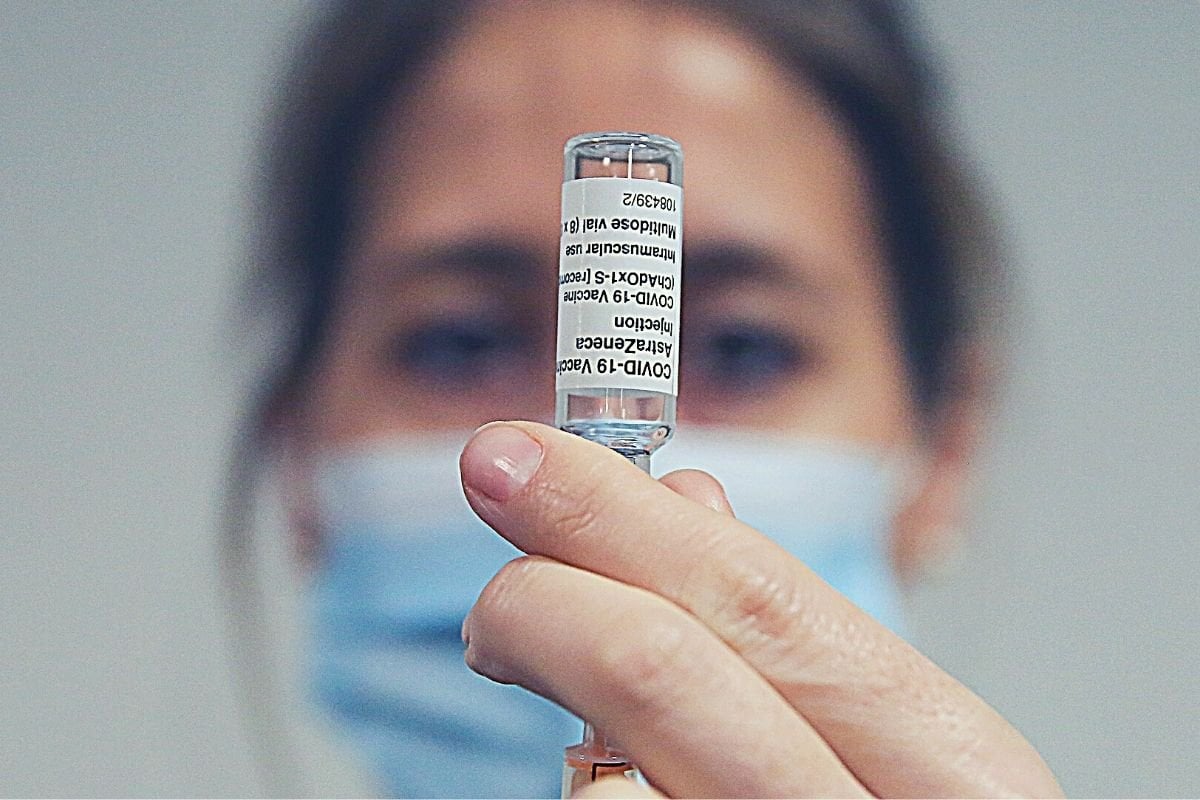
The change comes in the wake of a small number of global reports of blood clotting among recipients of the AstraZeneca vaccine — which is currently the only other COVID-19 jab approved for use in Australia.
So what's the risk posed by the AstraZeneca vaccine, and how will the new recommendation affect Australia's vaccine rollout? Let's take a look.
OK. So, what's changing exactly?
The Government has issued three new recommendations based on advice provided by The Australian Technical Advisory Group on Immunisation (a group of experts on vaccines, epidemiology and vaccination programmes):
- Pfizer is preferred over AstraZeneca COVID-19 vaccine in adults aged under 50 years;
- The AstraZeneca vaccine should only be given as a first dose to adults under the age of 50 where the benefit clearly outweighs the risk for that individual;
- People who have had their first dose of COVID-19 Vaccine AstraZeneca without any serious adverse effects can be given their second dose.
"It's a rare event, but it is serious"
— Sunrise (@sunriseon7) April 8, 2021
Chief Medical Officer Professor Paul Kelly on the government's decision to axe the AstraZeneca vaccine for Australians aged under 50 due to blood clot fears. pic.twitter.com/x2cGTEqOMF

