Content warning: This post deals with PTSD and suicidal ideation, and might be triggering for some readers.
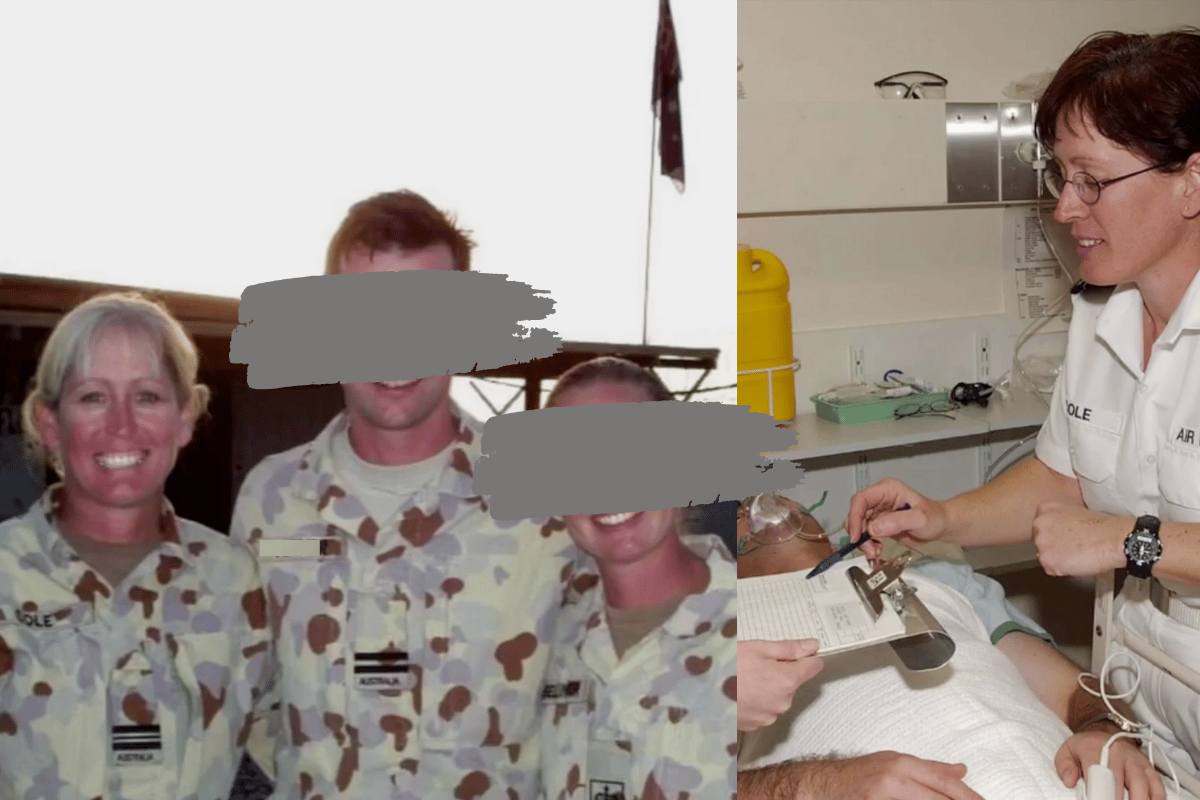
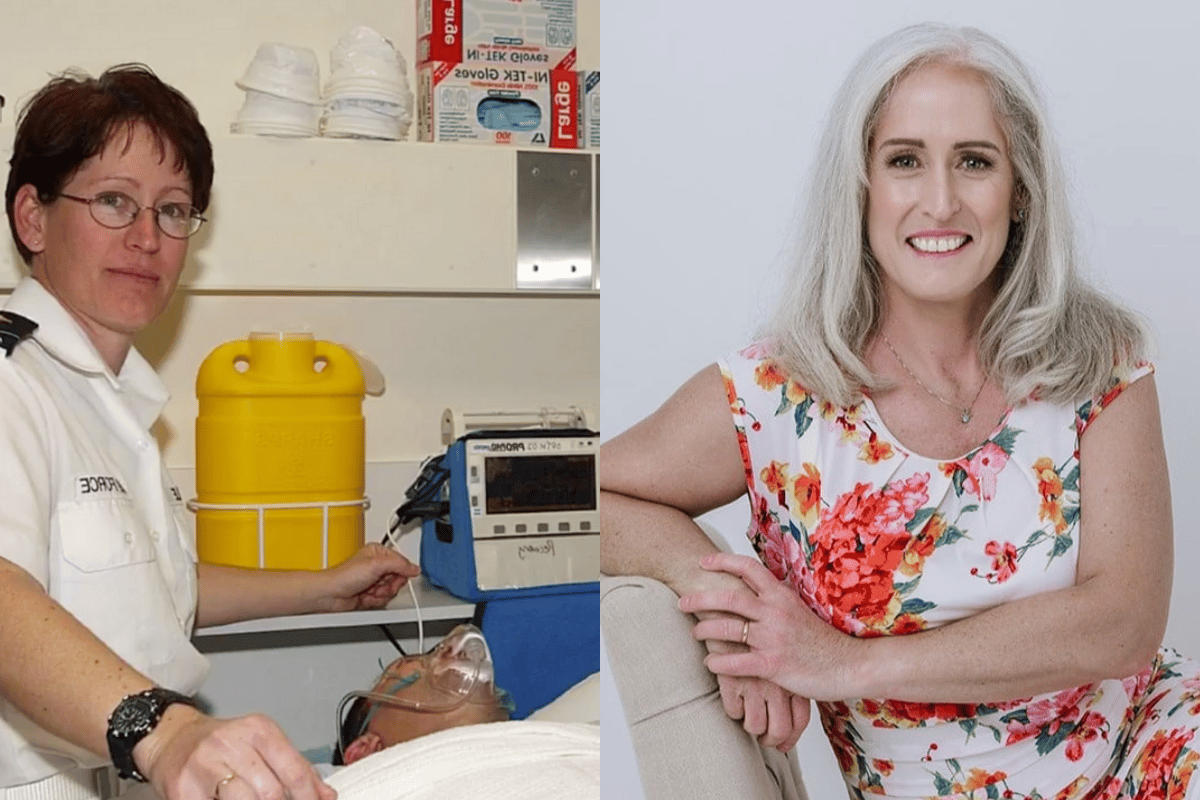
Michele Scherr knows all too well the horrors that war brings.
She spent almost 20 years as a Nursing Officer (Registered Nurse) with the Royal Australian Air Force.
And for those long years that Michele was a part of the Australian Defence Force (ADF), she was deployed to a number of high-risk operations, including in East Timor, Iraq and Afghanistan.
Watch: Debra Swain speaks about seeing signs of PTSD in her partner. Post continues below.
Initially, she was attracted to the challenge.
But as the years went on and the list of witnessing traumatic experiences grew longer, Michele was struggling.
You would imagine that working within a healthcare system while experiencing mental health issues would mean Michele would have access to support - knowing where to go and who to speak to.
But from her personal experience, she felt isolated, desperately requiring better support both from an organisational level and directly in the workplace.
And it left her in a vulnerable state.